Gage Johnson
Editor-in-Chief
[email protected]
Cady Stribling
News Writer
[email protected]
On Tuesday, Feb. 2, President Bob Jackson and a panel of distinguished medical, governmental and historical officials talked to the Murray State community about the latest COVID-19 updates and the vaccine at the first virtual Town & Gown President’s Breakfast of 2021.
Panelists included Chief Medical Officer Bob Hughes, CEO of Murray Calloway County Hospital Jerry Penner, Executive Advisor at the Kentucky Cabinet for Health and Family Services Mark Carter, Mayor Bob Rogers and history professor James Humphries.
In the forum, Carter said as of Monday, Feb. 1, a total of 362,271 people have been vaccinated in Kentucky with 86 percent of the first doses received administered. Carter said they were approaching Gov. Andy Beshear’s goal of having 90 percent of the doses received into arms within seven days.
Carter said patience is key since the biggest issue Kentucky currently faces is access to the vaccination. Kentucky otherwise has the healthcare system and distribution network in place to get the vaccine out.
There are currently two vaccines, the Pfizer and Moderna, both of which require two doses and involve complex ordering and transporting aspects, according to Beshear’s COVID-19 plan.
Carter said the Pfizer product, a two-dose vaccine given three weeks apart, requires special refrigeration in an ultra-cold storage at negative 60 to negative 80 degrees Celsius. Typically, only hospitals have this type of equipment, so the Pfizer vaccine is primarily being distributed to hospitals.
“When we get the vaccine in from the feds, we get about 25,000 doses,” Carter said. “When we ship it, because of the nature of the container and the need to keep it that cold, it’s shipped in lots of 975 doses. This makes it hard when you have to distribute it around. It has to go to large distribution sites.”
Penner said in the forum both the Pfizer and Moderna vaccines have 95 percent efficacy against the virus. There are also two additional vaccines “on the horizon,” Penner said. One is the Johnson & Johnson vaccine, a single dose that is still in test trials and is about 72 percent effective in the United States. Penner said the other is the Novavax, which is roughly 90 percent effective and currently in phase three of trials.
During the forum, Carter said Kentucky is expected to potentially receive over 60,000 doses by next week. Hypothetically, if the state receives 56,000 doses each week, Carter said it would take 16 months to vaccinate the entire state. The problem, then, comes back to access to the vaccine.
“As Bob (Hughes) indicated, when we get the vaccine, we’re going to put it in some arms,” Penner said. “I think we have some great plans to be able to do that. I know people ask questions about will we have the vaccine here and be able to get that. You know the real challenge… is trying to figure out when you have 1,100 people asking to be a vaccine site, where does it go? Where do we bring that into? So there are some tremendous challenges the state is dealing with right now, and they’re trying to roll it out as quickly as they can.”
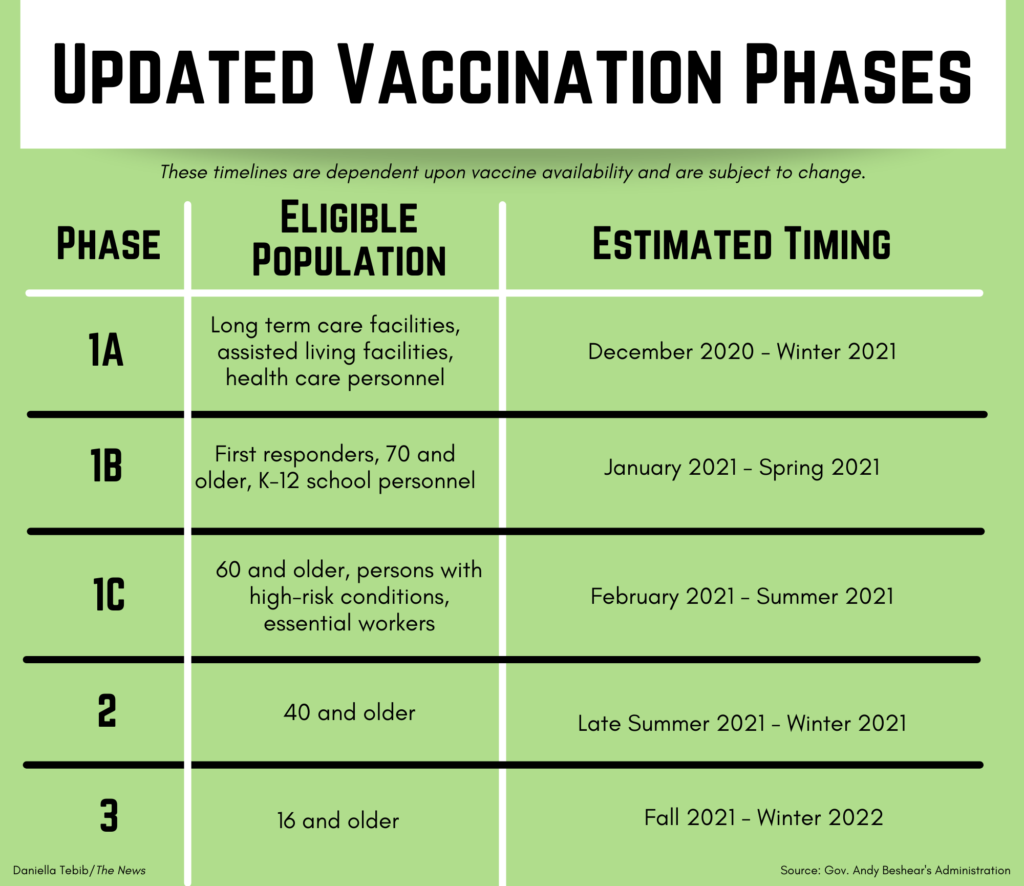
Kentucky is distributing the COVID-19 vaccine in phases, focusing on getting the vaccine to the most vulnerable members of society as quickly as possible, according to Beshear’s vaccine distribution plan.
Carter said distribution becomes a challenge in Kentucky because of the variation in size and population of counties, especially when the lowest population sits around 2,100 and the highest is 760,000. Allocation of vaccines could also change within a 24 hour period.
Penner said at Murray Calloway County Hospital the vaccines have been rolled out pretty quickly with many of the healthcare workers already getting their second doses.
Several questions were raised as to why Murray State was not included with the K-12 personnel in the 1B group to receive the vaccine. Jackson said postsecondary institutions such as Murray State have never been included in the K-12 category, which the University had been transparent in relaying.
Jackson said the Murray State community is included in group 1C under essential workers.
“This is not unique to Murray State,” Jackson said. “This was just a decision to get the frontline folks handled first, get our schools open, our K-12 schools open and really address those items as quickly as possible.”
Carter said people can still contract and test positive for COVID-19 even after receiving the vaccine but are not likely to experience severe symptoms. This also means people can still spread the disease to someone who hasn’t been vaccinated, Carter said.
“We need to keep doing these things of social distancing, taking care of our personal hygiene, wearing masks and getting vaccinated,” Carter said. “All of that needs to stay in place until we get to a point where we believe we have sufficient herd immunity, and that’s what’s going to make opening up the commonwealth’s schools, its businesses and getting our economy back to where it needs to be.”
Carter said he’s quoting local experts when saying the most important thing about the vaccine is that it prevents serious illness and death. With respect to these two issues, Carter said the vaccine is incredibly effective.

Hughes described his own experience receiving the first dose of the COVID-19 vaccine and testing positive for the virus not long after. In his case, Hughes consulted with a friend and colleague in the healthcare profession and was told to wait three months to receive the second dose of the vaccine. Hughes said if someone were to contract the virus after receiving the vaccine to consult their individual physician.
Hughes said there are encouraging studies showing an increased herd immunity causing lower case and death numbers. Carter said experts have varying opinions on herd immunity but estimate that at least 70 to 80 percent of Americans need to be vaccinated to achieve herd immunity. In Kentucky, Carter said approximately 2 to 2.4 million people need to be vaccinated, which accounts for children under 16 and folks who won’t take the vaccine.
Often asked about the various side effects someone might experience after the vaccine, Penner said at Murray Calloway County Hospital there was one person he knew of who had nausea, vomiting and other flu-like symptoms for 12-36 hours. Otherwise, it is possible people could experience a sore arm, a low-grade fever and chills.
Hughes said he is often asked many questions surrounding the vaccine changing the body’s ability to fight off other viruses or infections. He said it does not alter this ability nor does it change one’s DNA structure.
“The vaccine itself does not get in the nucleus of the cell, which is what determines what the cell is,” Hughes said in the forum. “It only affects the ribosome function part of the cell, which makes the proteins. It makes a spike look-alike that your own cells are creating so that when the virus comes in the body it’s sort of tricking it. The antibodies attack that virus thinking it’s that spike protein that your body did.”
Vaccine technology is 100 or more years old in the United States, Hughes said. When taking a typical vaccine, Hughes said people are always asked if they are allergic to eggs because they incubate it in what is essentially the yolk of a chicken. The COVID-19 vaccine, however, is different because it’s made in a chemistry lab with mRNA, making it a completely different technology.
“When it becomes available, I can only ask you to help us help you, and that’s by taking the vaccine,” Penner said. “It’s the most important thing we can do as we move forward in the fight against this particular virus. There is light at the end of the tunnel, and, you know, it’s going to start with that vaccine.”
Read more about Kentucky’s vaccination distribution plan, vaccination phases, vaccine monitoring statics and other frequently asked questions at kycovid19.ky.gov.
Find your specific vaccination phase, vaccine sites near your location and sign up for notifications about the vaccine once you are eligible at vaccine.ky.gov.
As of press time on Wednesday, Feb. 3, there have been 14 new confirmed cases, bringing the total number of confirmed cases to 3,229 with 3,036 recovered, 140 isolated at home, seven hospitalized and 46 deaths.
Hughes said there has been a decline in numbers lately because of the end of the “holiday surge,” not because the vaccine. It will take more time for the vaccine to cause a decline in case numbers.
Hospitals all across the region, however, have still faced major challenges. For example, Hughes said there are 87 patients in the hospital with four or five rooms available, and housing people becomes difficult if there’s a large admission day.
“Now this has been the norm for us in the last 60 days, and not just here but across the entire region,” Hughes said in the forum. “I meet with nine CEOs of the hospitals all the way down to Princeton on a weekly basis, and we talk about our situations. At one point, unbeknownst to the community, there were four ICU beds out of the four major hospitals in the area, including the two Paducah hospitals, the Mayfield hospital and Murray-Calloway.”
Penner said the significant spike in Murray’s COVID-19 case numbers happened after September. Typically, Penner said the hospital emergency department admits about 12 to 13 percent of patients, but over the last four months it has skyrocketed to over 20 percent. The increase in patients has caused a major strain on staff, Penner said. They have transferred patients to Bowling Green and Evansville, which was unheard of prior to the pandemic.
On Murray State’s campus, there have been eight confirmed cases for faculty and staff and 15 confirmed cases among students from January 31 to Wednesday, Feb. 3. The total number of total confirmed cases on campus since Jan. 4 is 53.
“The Murray State community did better than the [Murray] community as a whole,” Hughes said. “And that’s not a knock at the community as a whole, it’s just that the students did such a good job. And the faculty, the staff, with education, constant reminders and some enforcement. It’s amazing how well the campus did.”
Find more about Kentucky’s COVID-19 vaccine plan at kycovid19.ky.gov and vaccine.ky.gov.